It’s January and some of your clients in new Medicare Advantage plans give you a call. They’re not completely satisfied with their new plan.
As their insurance agent, you can inform them that they aren’t stuck with this coverage. Almost immediately after the Annual Enrollment Period (AEP), beneficiaries in Medicare Advantage plans have an option to reconsider their plan selection.
Your clients have the opportunity to enroll in a different plan that better suits them during the Medicare Advantage Open Enrollment Period (MA OEP).
Listen to this article:
Here’s what you need to know about Medicare open enrollment rules and the important do’s and don’ts that will keep you compliant.
Medicare Advantage OEP Qualifications
If your clients meet the following qualifications, let them know that they can change their coverage if they are not satisfied with the plan they selected.
The MA OEP is specifically for:
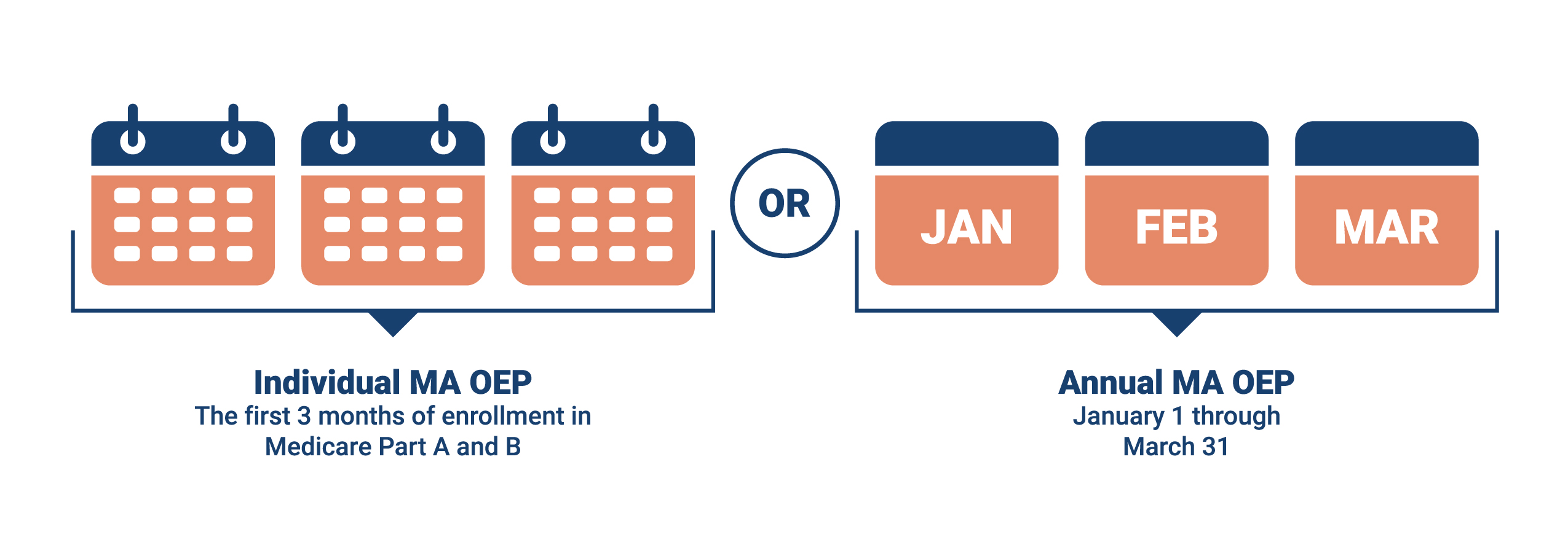
- Clients new to Medicare who enrolled in an MA plan during their Initial Coverage Election Period (ICEP). These beneficiaries have a three-month individualized OEP that starts with the month they are entitled to Part A and B. For example, if your client’s Part A and B eligibility begins June 1, then they have June, July, and August to make certain changes (explained below).
- Those who enrolled in MA plans as of January 1. For these clients, there is an OEP from January 1 to March 31.
This means that your clients calling you in January who are unhappy with their new plan can make a one-time switch in coverage. There are a few options for changing their coverage.
MA OEP Enrollment Cans & Can’ts
Here’s how a client can change Medicare plans during the OEP:
Remember the MA OEP was created for those with MA plans already. Your clients in Original Medicare or Med Supps can’t use OEP as an opportunity to enroll in an MA plan.
Part D changes are also limited and depend on changes to the MA plan. Clients can change their drug coverage by switching from one MAPD plan to another, by changing from an MA only to an MAPD plan, or by returning to Original Medicare and picking up a stand-alone Part D plan.
Those with Original Medicare and a Part D plan cannot switch to another drug plan during MA OEP. They’ll have to wait for an SEP or the next AEP.
Those with Original Medicare and a Part D plan cannot switch to another drug plan during MA OEP.
Marketing Do’s & Don’ts From MA OEP Rules
A big difference for agents between the AEP and the MA OEP is the restriction on marketing.
Agents cannot knowingly target or send unsolicited marketing materials to MA or Part D enrollees during the MA OEP (January 1 to March 31). It’s important to note that “knowingly” takes into account the intended recipient as well as the content of the message.
Note: If a beneficiary who has already made an enrollment decision unintentionally receives marketing information, it’s not considered “knowingly targeted.”
Here are some examples of things you cannot communicate to your clients concerning MA OEP.
- “Don’t like your new Medicare plan? Reach out to me about your disenrollment options.”
- “Did you know you can switch your MA plan from now until March 31? Let’s make an appointment.”
- “There’s limited time to make an appointment and switch plans.”
Effective Date of Coverage and Beyond
Coverage on a plan chosen during the MA OEP begins the first day of the month following the month an MA company gets the enrollment request. For example, if a client enrolls in a different MA plan on March 3, their new plan’s effective date would be April 1.
But note that the company in question can decide whether or not they’re open to enrollments during MA OEP, which means your clients are not guaranteed a plan during this period. Make sure you know which of the carriers you represent allow enrollments during MA OEP before making recommendations.
Make sure you know which of the carriers you represent allow enrollments during MA OEP before making recommendations.
That doesn’t mean your clients are stuck if this is the case. For instance, they may qualify for an SEP, so it’s possible their request for coverage will be accepted. If a client is able to change their coverage with an SEP, note that their coverage start date may be different.
Something to Think About
Before the MA OEP begins in January, reach out to your clients to make sure they understand their plans and that they are happy with them. Let them know you’re available if they have any questions or need further assistance. By doing so, you’ll provide your clients with a feeling of security, and as a result, they’ll be far more likely to refer their family and friends to you.
Remember, if you’re not contacting your clients throughout the year, another agent may seize the opportunity to gain their trust. A client who has questions or is confused with their plan is far more susceptible to allowing another agent write them into an MA plan next time around. Protect your business; don’t let the hard work you put into AEP go to waste.
For agent use only.





Not affiliated with or endorsed by Medicare or any government agency.
Share Post