On April 7, 2025, the Centers for Medicare & Medicaid Services (CMS) released the Final CY 2026 Part D Redesign Program Instructions. What’s changing with Part D for 2026?
As you’re likely well aware, CMS’ 2025 Part D Redesign brought several changes to the program to adjust to certain Inflation Reduction Act (IRA) provisions taking effect. Agents and beneficiaries alike will see more changes to the Part D program for 2026 that further the IRA’s implementation and possibly even alter it. Let’s take a look at what you should know!
Listen to this article:
2026 Part D Costs for Beneficiaries Announced
The exact costs associated with any kind of insurance coverage change each year. Budget-minded clients will appreciate knowing their future Part D costs, broken out below. You can also keep these costs in mind as you consider and discuss the impacts of enrolling in a Medicare Advantage Prescription Drug Plan (MAPD) versus Original Medicare and a stand-alone prescription drug plan (PDP) with your clients.
Part D Annual Deductible Increases $25
The standard 2026 Part D deductible will be $615, rising $25 from $590 in 2025. Though it is increasing again, it’s smaller than the $45 increase that occurred between 2024 and 2025.
Part D sponsors may choose to have a deductible lower than $615 or even none at all.
Beneficiaries will continue to pay 100 percent of their gross covered prescription drug costs until the deductible is met (if there is one).
Out-of-Pocket Threshold Increases $100
The 2026 Part D out-of-pocket threshold will be $2,100, rising from $2,000 in 2025. Beneficiaries will continue to pay 25 percent of their gross covered prescription drug costs until the out-of-pocket threshold is met.
After reaching the out-of-pocket threshold, clients will enter catastrophic coverage and will no longer pay additional out-of-pocket costs for prescription drugs.
The Selected Drug Subsidy Program Begins
Created in 2022 by the IRA, the Selected Drug Subsidy Program starts January 1, 2026. This change doesn’t directly affect beneficiaries, but it does indirectly affect them. We’ll explain…
The Selected Drug Subsidy program provides insurers with a government subsidy, equal to 10 percent of a selected drug’s negotiated price while a beneficiary is in the initial coverage phase. Theoretically, lowering insurers’ liability on the negotiated prices of selected drugs should help push beneficiaries’ costs down.
To qualify for the subsidy, the drug must be:
- A covered Part D drug that would be an applicable drug with respect to the Manufacturer Discount Program but for being a selected drug during a price applicability period
- Dispensed to an applicable beneficiary enrolled in a PDP or an MAPD plan who has not incurred costs that are equal to or exceed the annual out-of-pocket threshold
Note: Due to the first qualification criterion, drugs can only qualify for either the Selected Drug Subsidy Program or the Manufacturer Discount Program. No drug can qualify for both.
Two Slight Modifications to Part D Phases & Liabilities
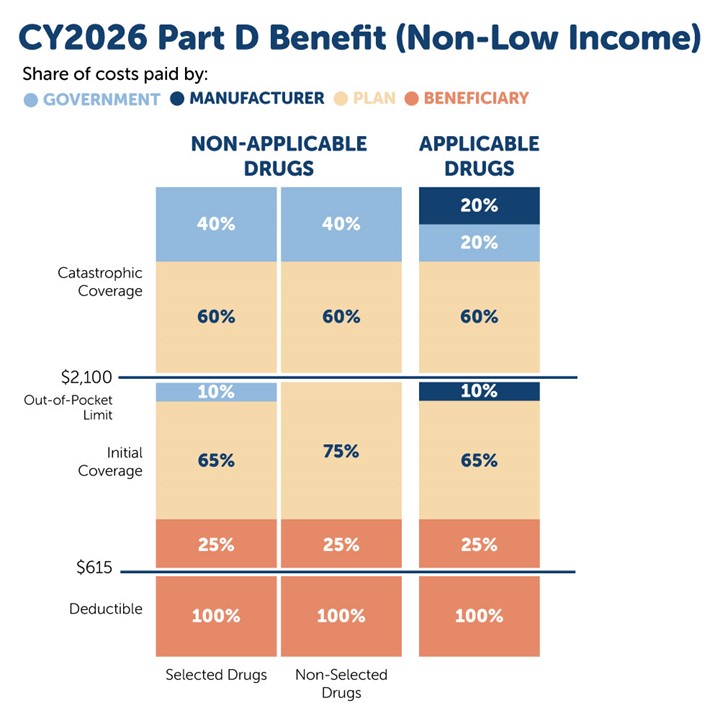
Generally speaking, the defined standard Part D drug benefit for 2026 will continue to consist of three phases. Two changes to the Part D benefit structure are highlighted in yellow.
-
Annual deductible:
-
The enrollee pays 100 percent of drug costs.
-
Once the enrollee meets the deductible (if applicable), they’ll enter the next phase.
-
-
Initial coverage:
-
The enrollee pays 25 percent coinsurance for covered Part D drugs.
-
The insurance carrier typically pays 65 percent of the cost of applicable drugs and 75 percent of the cost of all other covered Part D drugs.
-
Through the Manufacturer Discount Program, the drug manufacturer typically covers 10 percent of the cost of applicable drugs.
- CMS pays Part D insurers a 10 percent subsidy for selected drugs during a price applicability period.
-
Once the enrollee has reached the annual OOP threshold, they’ll move into the next phase.
-
-
Catastrophic:
-
The enrollee pays no cost-sharing for covered Part D drugs.
-
The insurance carrier typically pays 60 percent of the costs of all covered Part D drugs.
-
Through the Manufacturer Discount Program, the drug manufacturer typically covers 20 percent of the cost of applicable drugs.
-
CMS pays a reinsurance subsidy equal to 20 percent of the costs of applicable drugs and 40 percent of the costs of all other covered Part D drugs that are not applicable drugs, including selected drugs, during a price applicability period.
-
Here’s a visual representation of how the cost breakdown will change in 2026:
A Revised Simplified Determination Methodology for Part D Creditable Coverage
If you recall, in 2025, CMS revised the definition of creditable coverage and stated they were evaluating what creditable coverage determination methods to allow for 2026 and beyond. After considering the enhancements to the Part D benefit under the IRA, CMS has determined the current (“old”) simplified determination methodology “no longer reflects actuarial equivalence with defined standard Part D coverage.”
Starting in 2026, group health plans not applying for the retiree drug subsidy (RDS) can use a new simplified determination methodology. The methodology requires group health plans to pay at least 72 percent of each member’s prescription drug expenses.
CY 2026 will be the last year that non-RDS group health plans can use the old simplified determination method, which requires plans to pay 60 percent of each member’s prescription drug expenses.
See a detailed summary of the determination methods here
What This Means for Employers
Allowing plans to continue to use a simplified determination methodology should help keep group health plans affordable for Part D enrollees since it’s less labor intensive and costly for plans compared to the more complex actuarial determination method. By allowing group health plans access to the old simplified determination method for CY 2026, CMS hopes to minimize potential risks to the employer group market and plan members and ensure that all affected parties have time to implement to and adjust to the changes.
What This Means for Employees
It’s possible that Part D eligible employees with prescription drug coverage through their employer will see a change in their plan’s creditable coverage status.
Employers with health/prescription drug coverage are not required to offer creditable coverage to their employees. However, by law, employers must notify Part D-eligible plan participants of their plan’s creditable coverage status.
If the employee’s drug coverage becomes non-creditable, then they’ll have 63 days to change their coverage before they may be subject to a late enrollment penalty for Part D.
Medicare Prescription Payment Plan Updates Include Automatic Renewals
CMS’ 2026 Final Rule for MA & Part D codifies the Medicare Prescription Payment Plan (M3P) Program Instructions established by their final part one and two guidance PDFs, published in 2024, with a few modifications.
Starting next year, CMS will automatically renew the participation of enrollees in the program each calendar year unless an enrollee opts out. It’s worth making sure your clients who participate in M3P are aware they’ll be automatically re-enrolled in the program next year unless they tell CMS otherwise.
The Executive Order on Lowering Drug Prices
Apart from CMS’ Part D Redesign instructions, it’s important to note that President Donald Trump also recently signed an Executive Order that aims to reduce drug prices in the U.S. This order and the resulting actions government agencies and Congress take could affect the Part D program and beneficiaries in 2026 or future years.
Here’s a summary of what the order entails:
-
Prioritizing high-cost medications and transparency in the Medicare Drug Price Negotiation program
-
Aligning the treatment of small molecule prescription drugs with that of biological products for drug price negotiations (small molecule drugs have only nine years before the government can negotiate prices, while biologics have 13 years)
-
Aligning Medicare payments for drugs with those of hospitals and standardizing payment rates across different locations (“site-neutral payments”)
-
Encouraging states to import lower-cost drugs from Canada
-
Requiring that community health centers offer insulin and injectable epinephrine at significantly reduced prices to low-income and uninsured patients
-
Enhancing the disclosure of fees paid by pharmacy benefit managers and promoting a competitive drug value chain
Similar to 2025, we’ll see several Part D redesign changes in 2026. Some of these changes will be due to additional parts of IRA going into effect, and some could come about from the Trump Administration’s first year back in the White House. Time will only tell what all will happen, but we’ll strive to keep you updated if more changes are announced.
Stay up to date on the latest Part D and CMS changes. Register with Ritter for free!





Not affiliated with or endorsed by Medicare or any government agency.
Share Post