In 2025, CMS continues to adjust to the Inflation Reduction Act’s provisions, which aim to make prescriptions drugs more affordable to consumers, and their effects on the Part D market.
Review the most important 2025 Medicare Part D changes for your clients!
Want to stay up to date on Part D changes? Read our post on The 2026 Medicare Part D Redesign Updates Agents Should Know
2025 Part D Redesign Changes
On April 1, 2024, the Centers for Medicare & Medicaid Services (CMS) released the Final Calendar Year (CY) 2025 Part D Redesign Program Instructions, detailing CMS updates for Part D. What’s changed with Part D for 2025?
With a simplified structure, the CMS and IRA Part D redesign program updates fall into three main categories: updated beneficiary costs, restructured phases and liability (i.e., who pays and when), and modified TrOOP categories. Let'''s start by answering how much does Medicare Part D cost in 2025?
Beneficiary 2025 Part D Cost Updates
These Medicare changes demonstrate CMS’ continued implementation of the IRA, which eliminated the five percent coinsurance in the catastrophic phase in 2024.
Part D Annual Deductible Changes
The 2025 Part D annual deductible is $590 — a $45 increase from $545 in 2024. Some Part D sponsors may have a lower deductible or even none at all. Beneficiaries must pay 100 percent of their gross covered prescription drug costs until the deductible is met (if there is one).
Lower OOP Threshold
New for 2025, CMS has capped the Part D enrollee’s out-of-pocket (OOP) threshold at $2,000, which means clients don’t need to pay as much as in years past before entering the catastrophic coverage phase.
The Part D OOP threshold was $8,000 in 2024; however, this total included certain payments made on beneficiaries’ behalf. (For example, it included almost the full cost of brand-name drugs, including the manufacturer’s discount.) KFF reported Part D enrollees taking only brand-name drugs spent roughly $3,500 of their own money before reaching catastrophic coverage in 2024, so your clients could see savings of about $1,500 in 2025.
Restructured Part D Phases & Liabilities
In 2024, the Part D benefit consisted of four phases — annual deductible, initial coverage, coverage gap, and catastrophic coverage. CMS has eliminated the coverage gap phase for 2025, further ensuring the end of the donut hole era.
In this new, simplified structure, there are three phases, only two of which your client spends money in.
- Annual deductible:
- The enrollee pays 100 percent of drug costs.
- Once the enrollee meets the deductible (if applicable), they enter the next phase.
- Initial coverage:
- The enrollee pays 25 percent coinsurance for covered Part D drugs.
- The insurance carrier typically pays 65 percent of the cost of applicable drugs and 75 percent of the cost of all other covered Part D drugs.
- Through the Manufacturer Discount Program, the drug manufacturer typically covers 10 percent of the cost of applicable drugs.
- Once the enrollee has reached the annual OOP threshold of $2,000, they move into the next phase.
- Catastrophic:
- The enrollee pays no cost-sharing for covered Part D drugs.
- The insurance carrier typically pays 60 percent of the costs of all covered Part D drugs.
- Through the Manufacturer Discount Program, the drug manufacturer typically covers 20 percent of the cost of applicable drugs.
- CMS pays a reinsurance subsidy equal to 20 percent of the costs of applicable drugs and equivalent to 40 percent of the costs of all other covered Part D drugs that are not applicable drugs.
Here’s a visual representation of how the cost breakdown will change in 2025:
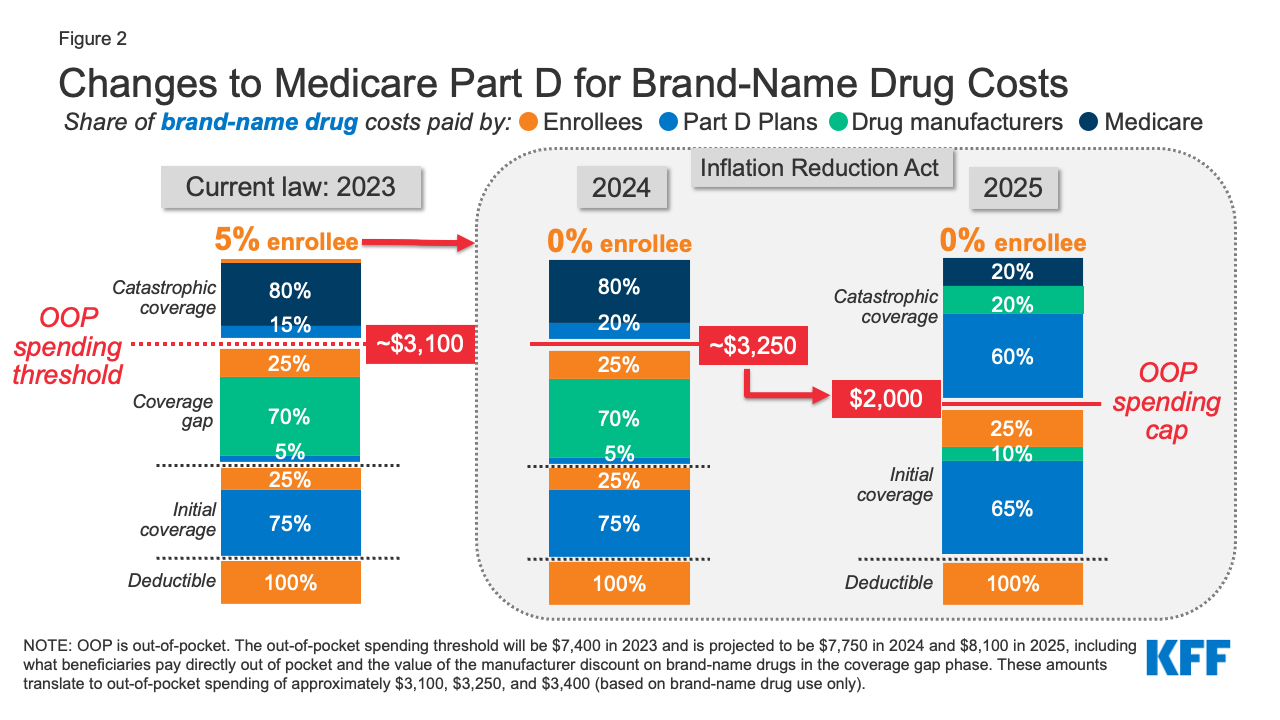
Source: KFF
CMS is phasing in the Manufacturer Discount Program for certain drugs of qualifying drug manufacturers over the next several years. The phase-in for the initial coverage phase will occur from 2025 through 2028 and that of the catastrophic phase will occur from 2025 through 2030. For any drug subject to the phase-in, Part D sponsors must pay the additional cost that would have otherwise been covered by the manufacturer discount.
Modified Medicare Part D TrOOP Categories
The IRA also updated what counts toward the True Out-of-Pocket Cost (TrOOP) for CY2025. TrOOP includes costs the beneficiary pays out of pocket for their prescriptions (e.g., their deductible, copayments, and coinsurance) along with select other payments made on a beneficiary’s behalf (e.g., State Pharmaceutical Assistance Program payments, AIDS Drug Assistance Programs). Premium payments do not count toward TrOOP.
For 2025, TrOOP:
- Includes: Payments for previously excluded supplemental benefits provided by Part D sponsors and Employer Group Waiver Plans (EGWPs)
- Excludes: Payments under the new Manufacturer Discount Program
Previously, payments under the Medicare Coverage Gap Discount Program counted toward TrOOP. That program has been replaced by the Manufacturer Discount program.
Since TrOOP determines when your client enters the initial coverage phase, qualifies for the Manufacturer Discount Program, reaches the annual OOP threshold, and enters the catastrophic coverage phase, these changes may affect the speed with which your client moves through coverage phases.
A New Medicare Prescription Payment Plan
Although your clients’ OOP costs should be lower this year, they could still owe up to $2,000 out of pocket. New for 2025, Part D enrollees can now manage these costs in the form of capped monthly payments. The Medicare Prescription Payment Plan means your clients don’t have to pay upfront and in full at the pharmacy for their covered drugs.
Learn more about the Medicare Prescription Payment Plan in our blog post on the subject, Preparing Clients for the New Medicare Prescription Payment Plan Program
Manufacturer Discount Program
This year, CMS officially sunset the Medicare Part D Coverage Gap Discount Program (CGDP) and established the Manufacturer Discount Program (Discount Program) — a necessary move due to elimination of the coverage gap phase.
Essentially, the IRA reorganized liability between the manufacturer and Part D sponsors and shifted more liability to the manufacturer and away from Medicare in the catastrophic phase. Manufacturers now cover 10 percent for all applicable drugs in the initial coverage phase and 20 percent of all applicable drugs in the catastrophic phase. Certain specified and small manufacturers will follow a discount phase-in period over the next five years.
Here’s how the Discount Program will work with the deductible:
- If a beneficiary doesn’t satisfy their plan’s deductible but meets TrOOP to satisfy the defined standard deductible:
- They are an applicable beneficiary under the Discount Program and deemed to have satisfied their plan deductible.
- If the beneficiary does satisfy the plan’s deductible or utilizes a drug not subject to the deductible but is not eligible for the Discount Program because they have not incurred sufficient TrOOP-eligible costs to satisfy the defined standard deductible amount:
- The Part D sponsor must cover the portion of costs a manufacturer would have owed had Discount Program discounts begun.
- Your clients don’t owe more than their deductible and 25 percent coinsurance in the initial coverage phase. Instead, their plan covers any remaining portions.
Unlike under the Coverage Gap Discount Program, manufacturer discounts under the new program are available regardless of whether or not the Part D enrollee is entitled to a low-income subsidy, and discounts do not count toward the enrollee’s incurred costs. The applicable discount is not available until the enrollee has incurred costs exceeding the annual deductible, regardless of whether the enrollee pays the deductible through assistance.
For all the details, see CMS’ Manufacturer Discount Program Final Guidance.
Part D Creditable Coverage Determination Changes
CMS has revised the definition of creditable coverage to exclude discounts paid under the Manufacturer Discount Program when determining the actuarial value of the standard Part D benefit and a plan sponsor’s plan. This value should be based on the amount the plan pays and includes the federal reinsurance subsidy in the catastrophic phase.
Additionally, while draft guidance suggested the simplified determination methodology would no longer be available for 2025, CMS is continuing to allow plans to use it for CY2025 and will continue to allow plans to use it for CY2026. However, for CY2026, they’re introducing a revised simplified determination methodology and sunsetting the “old” simplified determination method for 2027.
In general, these changes put a burden on group health plans to balance benefit enhancements with affordability.
In general, these changes put a burden on group health plans to balance benefit enhancements with affordability. Clients may need help navigating coverage to avoid a late enrollment penalty.
Learn more about the Part D creditable coverage determination changes and their impact
The New Part D Premium Stabilization Demonstration Program
On July 29, 2024, while announcing preliminary 2025 Medicare Part D bid information, CMS simultaneously announced the creation of a new premium stabilization program to help subsidize the cost of Part D for prescription drug plans as IRA changes take effect.
Plan participation in this new program could lead to smaller increases in PDP premiums than would happen otherwise.
As of now, it’s unclear if the Trump Administration will continue to implement this program.
The Future of Part D
AWith more parts of the IRA being implemented down the road and 2025 ushering in a new presidential administration, we’ll likely see additional changes to the Medicare market. Some of those upcoming Part D changes, like CMS’ 2026 Part D redesign updates, are already known. Others may be yet to be announced.
No matter the unknown, as Part D continues to evolve, we’ll all need to adapt along with it.
Prescription drug plans are still an important component to your portfolio, especially if you sell Medicare Supplements. Download our free guide to learn more about selling Part D insurance plans.







Not affiliated with or endorsed by Medicare or any government agency.
Share Post