Attention Illinois, Michigan, and Ohio insurance agents! Your states’ new Medicaid contracts are shaking up insurers’ Dual Eligible Special Needs Plan (D-SNP) market share and presenting new opportunity in the Midwest.
If you want to grow your business in IL, MI, or OH, we believe now’s the time to make a few strategic moves to understand and sell D-SNPs. Keep reading for a brief overview of the D-SNP market in the Midwest and our agent sales advice!
Strategize for More Sales
Just registered and ready to unlock fully online contracting through Contract Now? Have a conversation with your sales specialist.
What’s Happening with the Dual Eligible Market in the Midwest?
Generally speaking, after guidance from the federal government, U.S. states and insurers are transitioning to integrated D-SNPs to better coordinate care, control costs, and protect consumers. For local-market details, find your state below.
Illinois D-SNP Awards & Changes for 2026
At the end of 2024, the Illinois Department of Healthcare and Family Services (HFS) put all their Medicaid managed care contracts up for rebidding due to CMS ending the capitated care model in the federal Financial Alignment Initiative demonstration program.
Current Illinois Medicare-Medicaid Alignment Initiative (MMAI) demonstration contracts were last awarded in 2017 to CVS/Aetna, Blue Cross Blue Shield of Illinois, Humana, Centene/Meridian Health Plan, Molina Healthcare, and Cook County’s CountyCare Health Plan. They expire December 31, 2025. New Illinois D-SNP contracts were recently awarded to Aetna Better Health, Humana Health Plan, Meridian Health Plan, and Molina Healthcare. They will run January 1, 2026, through December 31, 2029, within the state’s new Fully Integrated Dual Eligible Special Needs Plan (FIDE-SNP) model. After December 31, 2029, these Medicare-Medicaid contracts may be extended for up to five years and six months.
New Illinois D-SNP contracts were recently awarded to Aetna Better Health, Humana Health Plan, Meridian Health Plan, and Molina Healthcare.
Illinois’ current MMAI program serves about 80,000 dual eligibles. Starting in 2027, its D-SNPs will also manage long-term services and supports (LTSS), which is currently run under a separate program with around 60,000 beneficiaries enrolled. Dual eligibles who receive those services will be required to enroll in managed care, unless they have a valid exception (e.g., receives institutional services for developmental disabilities), per the FIDE-SNP model.
Did you know? Approximately 399,629 Illinoisians are dual eligibles.
Michigan D-SNP Awards & Changes for 2026
The Michigan Department of Health and Human Services (MDHHS) announced it will provide a new benefit plan for dual eligibles, MI Coordinated Health, starting January 1, 2026, in select counties. In part, they’ve updated D-SNP contract awards for Michigan’s nine health plans, including:
- Aetna Better Health of Michigan Inc.
- AmeriHealth Michigan, Inc.
- HAP CareSource
- Humana Medical Plan of Michigan, Inc.
- Meridian Health Plan of Michigan, Inc.
- Molina Healthcare of Michigan, Inc.
- Priority Health Choice, Inc.
- UnitedHealthcare Community Plan, Inc.
- Upper Peninsula Health Plan, LLC
The contracts are region-specific and will run for seven years, offering three potential one-year extensions after that. They will operate within Michigan’s new Highly Integrated Dual Eligible Special Needs Plan model (HIDE-SNP).
MI Coordinated Health will be available in the following regions starting January 1, 2026:
- Region 1 — Upper Peninsula Prosperity Alliance
- Region 8 — Southwest Prosperity Region
- Region 10 — Detroit Metro Prosperity Region — Macomb
- Region 10 — Detroit Metro Prosperity Region — Wayne
2026 Integrated D-SNP Carrier Availability in MI by Region
Source: https://www.michigan.gov/mdhhs/inside-mdhhs/newsroom/2024/12/06/mi-coordinated
It will also be available in the following regions starting January 1, 2027:
- Region 2 — Northwest Prosperity Region
- Region 3 — Northeast Prosperity Region
- Region 4 — West Michigan Prosperity Alliance
- Region 5 — East Central Michigan Prosperity Region
- Region 6 — East Michigan Prosperity Region
- Region 7 — South Central Prosperity Region
- Region 9 — Southeast Prosperity Region
- Region 10 — Detroit Metro Prosperity Region — Oakland
2027 Integrated D-SNP Carrier Availability in MI by Region
*Coverage newly available January 1, 2027
Source: https://www.michigan.gov/mdhhs/inside-mdhhs/newsroom/2024/12/06/mi-coordinated
Michigan currently offers MI Health Link, a program which will expire at the end of 2025.
Did you know? Approximately 334,716 Michiganders are dual eligibles.
Ohio D-SNP Awards & Changes for 2026
Starting January 1, 2026, Ohio is welcoming Next Generation changes to its MyCare program for dual eligibles. The Ohio Department of Medicaid (ODM) awarded 2026 Medicaid contracts to Anthem Blue Cross and Blue Shield, Buckeye Health Plan, CareSource, and Molina Healthcare of Ohio for the program. Moving forward, the state will utilize a FIDE-SNP model, and coordination-only D-SNPs will no longer be permitted. Adults must now be 21 years or older to qualify, whereas they used to only have to be at least 18.
Next Generation MyCare plans will roll out via a two-phase approach. The first phase will provide access to the new plans in the 29 counties where the MyCare program currently runs. In the second phase, the new plans will become available statewide over a several-month planned expansion.
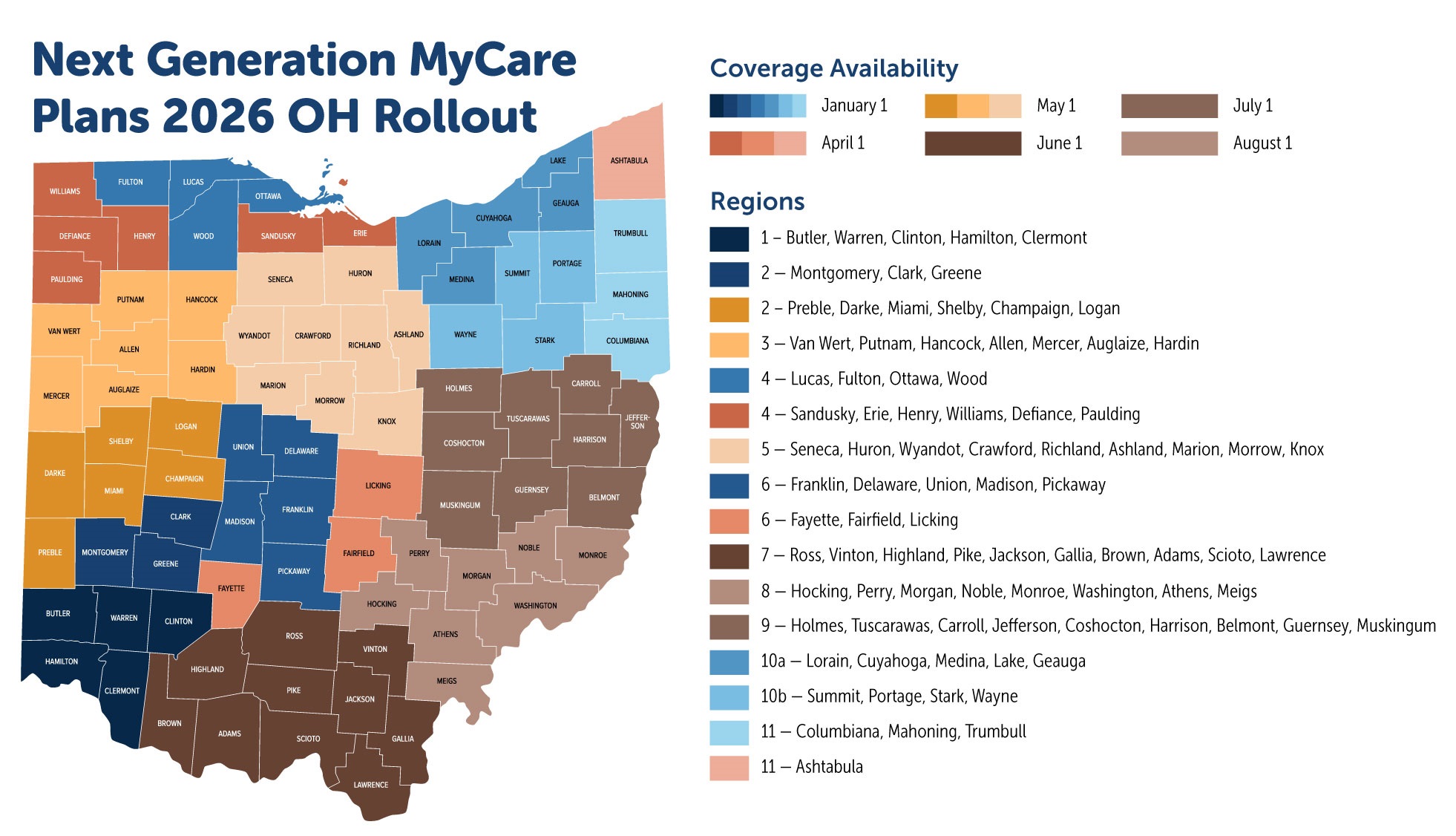
Where Next Generation MyCare plans will be available starting January 1, 2026:
- Region 1 — Butler, Warren, Clinton, Hamilton, Clermont
- Region 2 — Montgomery, Clark, Greene
- Region 6 — Franklin, Delaware, Union, Madison, Pickaway
- Region 4 — Lucas, Fulton, Ottawa, Wood
- Region 10a — Lorain, Cuyahoga, Medina, Lake, Geauga
- Region 10b — Summit, Portage, Stark, Wayne
- Region 11 — Columbiana, Mahoning, Trumbull
Where Next Generation MyCare plans will also be available starting April 1, 2026:
- Region 4 — Sandusky, Erie, Henry, Williams, Defiance, Paulding
- Region 6 — Fayette, Fairfield, Licking
- Region 11 — Ashtabula
Where Next Generation MyCare plans will also be available starting May 1, 2026:
- Region 2 — Preble, Darke, Miami, Shelby, Champaign, Logan
- Region 3 — Van Wert, Putnam, Hancock, Allen, Mercer, Auglaize, Hardin
- Region 5 — Seneca, Huron, Wyandot, Crawford, Richland, Ashland, Marion, Morrow, Knox
Where Next Generation MyCare plans will also be available starting June 1, 2026:
- Region 7 — Ross, Vinton, Highland, Pike, Jackson, Gallia, Brown, Adams, Scioto, Lawrence
Where Next Generation MyCare plans will also be available starting July 1, 2026:
- Region 9 — Holmes, Tuscarawas, Carroll, Jefferson, Coshocton, Harrison, Belmont, Guernsey, Muskingum
Where Next Generation MyCare plans will also be available starting August 1, 2026:
- Region 8 — Hocking, Perry, Morgan, Noble, Monroe, Washington, Athens, Meigs
Ohio’s MyCare program, expiring at the end of 2025, started in 2015. Currently, Aetna, Buckeye, CareSource, Molina Healthcare, and UnitedHealthcare participate in the program.
Did you Know? Approximately 401,459 Ohioans are dual eligibles.
Strategizing Your Dual Eligible Special Needs Plan Sales in the Midwest
If you’re selling health insurance, D-SNPs should already be part of your portfolio. If they aren’t, you can read why you should sell D-SNPs here. Either way, we believe it’s critical that agents in the Midwest who want to increase their sales and help more clients into the best coverage take these three steps now.
It’s critical that agents in the Midwest who want to increase their sales and help more clients into the best coverage take three steps now.
1. Increase Your Understanding of D-SNPs
There were a lot changes to the D-SNP market for 2025 from the federal government. As we discussed above, there were many state-level adjustments to the market as well. If you have already been selling D-SNPs in IL, MI, and OH, make sure you’re up to speed on what’s new. The website for your state’s Department of Medicaid can be a great place to find links to more info on their specific program updates:
If you’re not sure how D-SNPs work, such as their plan structure, enrollments, effective dates, etc., check out our free D-SNP sales training eBook or read our beginner’s guide to D-SNPs blog post! Our Sales team is also here to help you with any general or state- and county-specific questions you may have!
Download Ritter’s Complete Guide to Selling D-SNPs eBook — featuring cheat sheets, a glossary, and a checklist to help streamline sales!
2. Contract with 2026 Integrated D-SNP Carriers in Your State
You have the knowledge; make sure you also have contracts with the carriers that have been awarded new Medicaid contracts in your state to offer their plans during qualifying Open and Special Enrollment Periods!
Uniquely, Ritter offers fast online contracting with the carriers below via our Contract Now tool. To unlock online contracting or ask for information, register with our site first (it’s free and only takes about a minute) and then speak with your sales specialist (to verify you’re not a bot and get even more targeted plan recommendations). Registering with our site also gives you free access to Ritter sales tools, including a quote engine, client-facing website, and customer relationship management system!
While 2026 details are not available yet, partnering with these carriers now streamlines the process once the new products become available.
“Note, Molina Healthcare will be one of only two carriers that offer integrated D-SNPs across all three states — IL, MI, and OH! I believe there’s a huge opportunity to grow with this carrier, and I’d recommend contracting with Molina Healthcare now.” — Lincoln LaFayette, President of Quick Insured Brokerage
Illinois D-SNP Contracting
- Aetna Better Health | Contract now | Learn more
- Humana Health Plan | Contract now | Learn more
- Meridian Health Plan | Contract now |Learn more
- Molina Healthcare | Contract now | Learn more
Note: Meridian Health Plan is owned by Centene/Wellcare.
“Molina’s MAPD/D-SNP market share is less than one percent statewide, but it will grow with the loss of Blue Cross Blue Shield of Illinois and Cook County’s CountyCare Health Plan. Make sure they’re at least in your portfolio for IL!” — Lincoln LaFayette, President of Quick Insured Brokerage
Michigan D-SNP Contracting
- Aetna Better Health of Michigan Inc. | Contract now | Learn more
- AmeriHealth Michigan, Inc. | Contract now | Learn more
- HAP CareSource | Contract now | Learn more
- Humana Medical Plan of Michigan, Inc. | Contract now | Learn more
- Meridian Health Plan of Michigan, Inc. | Contract now |Learn more
- Molina Healthcare of Michigan, Inc. | Contract now | Learn more
- Priority Health Choice, Inc. | Contract now | Learn more
- UnitedHealthcare Community Plan, Inc. | Contract now | Learn more
- Upper Peninsula Health Plan, LLC | Learn more
Note: Our AmeriHealth MAPD contract is under Independence in Contract Now. Select IBC — AmeriHealth Medicare for the proper plan year. Meridian Health Plan of Michigan, Inc. is owned by Centene/Wellcare.
“Remember, Michigan integrated D-SNPs will be available in select counties for 2026 and statewide for 2027. If you’re in Region 1, you’ll need Upper Peninsula Health Plan, though we don’t currently offer contracting. Meridian, Molina Healthcare, Priority Health, and UnitedHealthcare will offer plans in all other regions across the state. Humana, Aetna, HAP/Caresource, and AmeriHealth will offer plans in select regions.” — Lincoln LaFayette, President of Quick Insured Brokerage
Ohio D-SNP Contracting
- Anthem Blue Cross and Blue Shield | Contract now | Learn more
- Buckeye Health Plan | Contract now | Learn more
- CareSource | Contract now | Learn more
- Molina HealthCare of Ohio | Contract now | Learn more
Note: Buckeye Health Plan is owned by Centene/Wellcare.
“Ohioans will only have access to four FIDE carriers in 2026; Molina Healthcare, Wellcare, Anthem, and CareSource. If these carriers aren’t in your portfolio already, add them today.” — Lincoln LaFayette, President of Quick Insured Brokerage
3. Help More Clients & Earn More Commissions
The market and plan shake-ups are coming. Some people will lose existing coverage and need new D-SNP coverage. Others will newly qualify for D-SNPs. And yet others won’t qualify for D-SNPs anymore at all. There will be people with questions. Set yourself up to provide the answers, then go forth and provide them!
We can’t promise your success, but if you’re the go-getter we believe you are, understanding and selling D-SNPs in IL, OH, and MI for 2026 should lead you to help even more clients and earn more commissions.
States in the Midwest are updating their Medicaid programs for 2026, and future years, now. As a result, market share for D-SNP insurers awarded contracts by state governments will be up for grabs. Follow our three steps, and you should be ready to know, go, and grow!






Not affiliated with or endorsed by Medicare or any government agency.
Share Post