The 2026 marketplace ACA Open Enrollment Period (OEP) runs November 1, 2025, to January 15, 2026 (can vary in some state-based marketplaces). This is the most crucial time for your clients who are under 65 and in need of Affordable Care Act health insurance coverage.
Below are some things to know before assisting clients with finding coverage this OEP. First, we’ll discuss important changes you should know before diving into the nitty gritty!
Need help getting ready-to-sell on the federal or state exchanges? Learn more about how to prepare for the OEP
What’s New This OEP?
The 2025 ACA Marketplace Integrity and Affordability Final Rule introduced new income and eligibility verification requirements and a $5 monthly premium charge for those who don’t owe a premium due to Advanced Premium Tax Credits (APTC) and who do not actively renew.
Legislation such as The One Big Beautiful Bill Act (OBBB) has also influenced who’s eligible for ACA coverage and these premium tax credits.
Stringent Medicaid requirements introduced by the bill could lead to more individuals looking for ACA plans. With the discontinuation of auto renewals, your clients will need to make sure they verify their incomes to remain covered. In addition, consumers who enroll in a plan using a non-qualifying life event (QLE) Special Enrollment Period (SEP) won’t receive premium tax credits or Cost Sharing Reductions (CSRs) starting in Plan Year 2026.
Make sure your clients know that if their estimated income was lower than their actual income, the extra of the premium tax credits will now be reclaimed in full regardless of the household income!
Note: The OBBB did not extend pandemic-ERA enhancements to ACA subsidies. As of now, the ACA subsidy cliff continues to approach and enhancements are set to expire at the end of the year.
Any of these updates may change at any time.
Collect Your Clients’ Demographic Information
To determine what types of plans will work best for your client, collect their demographic details. This includes where they live, their household income, and the sex and age of all applicants. Household incomes determines whether your client is eligible for premium tax credits, or subsidies. The number of applicants is important to note if you have more than one individual signing up for coverage. As their agent, you must provide information about anyone on your client’s tax return. This includes people who do not live in the same household, as well as those who are not enrolling in the coverage.
You must also provide this for anyone under 21 who lives in the household with your client. This applies even if they are not a tax dependent.
Where your client lives can affect what health coverage they are eligible for. For example, some states have their own exchanges and others participate in the federal exchange. Become familiar with the right exchange for your client to identify where they need to register for coverage.
Collecting this basic information is the first step to finding affordable health care options for your clients in need.
How to Find Providers Available in Your Clients’ Area
After choosing the right exchange to find a plan, the next step is to find the main hospital systems in your clients’ area. It can be helpful to understand which carriers participate with which hospital systems.
You can find which hospital systems are active in your clients’ area by searching carriers’ websites for specific providers.
If you use an enrollment platform like HealthSherpa, you can click the direct links to the carrier page. There, you can use their provider search tool.
Currently, HealthSherpa works for the federal exchange as well as Georgia. Many state-based marketplace enrollment sites will allow you to access provider search tools as well.
Enhanced Direct Enrollment (EDE) tools such as HealthSherpa can be helpful to enroll clients and manage their plan in one platform. Creating an account is free and helps to streamline the enrollment process. Register with Ritter today and use our FB05 join code to link to our HealthSherpa account. Doing so gives us access to assist with your account if you need it.
We recommend searching for hospital systems for each client. Consider their preferences or specific health needs when identifying the carrier and network that’s right for them.
Make sure you communicate with your clients throughout this process to ensure that their needs are being met. If your client has a primary care provider (PCP) that in the plan’s network, think about that plan for their marketplace coverage.
Make sure you communicate with your clients throughout this process to ensure that their needs are being met.
What Plan Options Are Available?
Insurance carriers offer many different types of ACA plans. Three different plan types exist: Health Maintenance Organization (HMO), Preferred Provider Organization (PPO), and Exclusive Provider Organization (EPO).
HMO & EPO plans limit coverage to a local network of physicians and facilities. They usually will not cover out-of-network care, except for emergency services.
PPO plans have a larger medical provider network and will cover costs out-of-network but for a higher premium.
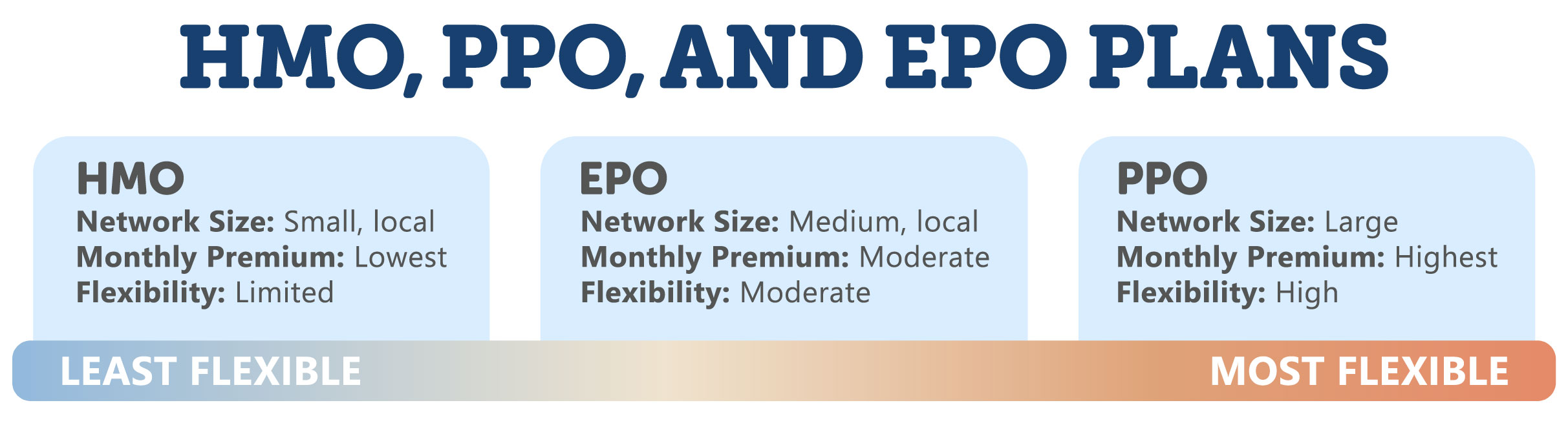
HMO plans can require a referral from a PCP to see a specialist, while PPOs and EPOs do not. Because of this, some individuals may choose an EPO or PPO plan for added flexibility.
However, these more flexible plans are also more expensive. Consider both flexibility in network and affordability when your client is choosing a plan.
In addition to the three plan types, there are four metal tiers: bronze, silver, gold, and platinum. These tiers separate how medical costs are shared between the policy and the beneficiary.
The levels do not describe the quality of care or the services that are covered by the insurance provider. The table below shows the basic structure of the four metal tiers.
The Metal Tiers for ACA Health Plans
| Tiers | Bronze | Silver | Gold | Platinum |
|---|---|---|---|---|
| % Covered Medical Costs Paid by the Policy | 60% | 70% | 80% | 90% |
| % of Covered Medical Costs Paid by the Policyholder | 40% | 30% | 20% | 10% |
| Monthly Premium Comparative Cost | Lowest | Moderate | High | Highest |
| Unsubsidized Annual Deductible Comparative Cost | Highest | Moderate | Low | Lowest |
| Eligible to Apply a Cost-Sharing Reduction? | No | Yes | No | No |
| Eligible to Apply a Premium Tax Credit? | Yes | Yes | Yes | Yes |
The table shows that, as the metal tiers increase, a member’s coinsurance responsibility decreases. The most common tier in the marketplace is silver. In this tier, clients can apply a premium tax credit to reduce costs.
Download our handout Understanding the ACA Metal Tiers for a quick reference during your client appointments this OEP!
When Coverage Will Begin
To start coverage, help your clients successfully complete their application. Then, direct them to pay the first monthly premium.
Here’s how your clients can access their account (in FFM states):
- Log in to HealthCare.gov.
- Select the application under Your Existing Applications.
- Click the blue button that says Pay Your First Health Insurance Monthly Premium.
- If online payment is available, select the green button Pay for Health Plan Now to go to the insurance company’s website to pay.
Alternatively, your client can use HealthSherpa in an FFM state. Quoting and enrolling in state-based exchange states must be done through that state’s unique exchange.
Some insurance companies do not participate in online payment. In this situation, the carrier will contact your client about next steps.
In most cases, for the 2026 plan year, coverage will begin on January 1 for plans enrolled in from the start of OEP through December 15. Coverage will begin on February 1 for plans enrolled from December 16 through January 15.
Effective dates can vary between exchanges. For example, some states may have an extended OEP, allowing a client to sign up for ACA coverage as late as January 31 and have an effective date of March 1. Ensure the correct effective date for your clients’ correct exchange and plan and advise them when their coverage will begin.
Starting in 2027, all OEPs must begin by November 1. They must end no later than December 31 and last no longer than nine weeks.
For the federal OEP, starting in 2027, the OEP will be November 1 through December 15. After PY2027, the effective dates will become standardized back to January 1.
In FFM states, verify that your clients’ coverage is active by signing into HealthCare.gov and checking under My Plans and Programs. (You can also check your clients’ coverage through HealthSherpa or the appropriate state-based exchange.)
For health plans that were signed up for during the beginning of the OEP, most coverage will begin January 1, 2025.
What Happens If Your Client Misses the OEP?
If you and your client miss the OEP, there could be other options to access affordable health care through the marketplace. In case of significant changes, your client may be eligible for a Special Enrollment Period (SEP).
Life changes, like having a baby, moving to a location where the plan is not available, or losing access to credible health insurance can qualify an individual for an SEP to enroll in a marketplace insurance plan. An SEP is the only way to register for marketplace coverage outside of the OEP.
Verify that the application information is correct, including the information that qualifies your client for an SEP. Your client may be asked to provide additional documentation to confirm eligibility based on the life event experienced.
If your client is can’t get an SEP, they may still need health care coverage. Consider a short-term medical policy, if it is available. This is an option for clients that can pass health underwriting.
They can get coverage for a short time, but the time varies depending on the state. Some states allow for 12-month or tri-term plans. Others, like Ritter’s home state of Pennsylvania, follow the three months with a one-month extension. These plans do not meet ACA rules, but they are a great option for your clients who need them.
The OEP is a crucial time for your clients under 65 who are looking to sign up for a marketplace plan.
Your clients are counting on you to guide them through the process. These essentials will allow you to prepare your clients for enrolling in their new marketplace insurance plan.
Ritter is committed to keeping our agents in the know. Register with our site to stay informed.






Not affiliated with or endorsed by Medicare or any government agency.
Share Post